Diabetes – Diabetic Retinopathy
 by Stephen G. Schwartz, MD, MBA
by Stephen G. Schwartz, MD, MBA
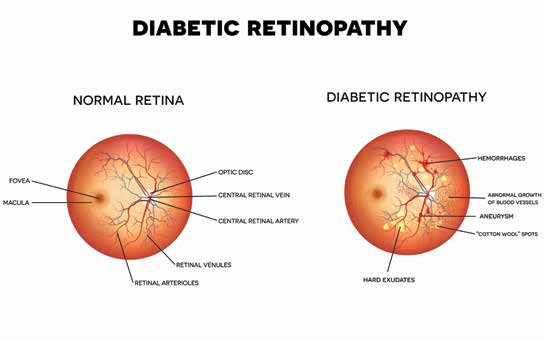
Diabetes is a common condition in which high blood sugar causes damage to blood vessels throughout the body, including the heart, kidneys, nerves, and eyes. This type of injury to blood vessels in the retina is called diabetic retinopathy, which is the leading cause of blindness in working age Americans. In the retina, which is the tissue that lines the back of the eye, blood vessels can be viewed directly. By dilating the pupil, your retina specialist is able to examine the retina for signs of damaged blood vessels and gain information about the status of diabetes throughout your body.
A healthy retina is necessary for good vision. Diabetic retinopathy can cause permanent vision loss not correctable by glasses.
All people with diabetes are at risk for developing diabetic retinopathy. The duration of diabetes and the extent of blood sugar, blood pressure, and cholesterol control are the most important risk factors for developing this potentially devastating condition. The Diabetes Control and Complications Trial (DCCT) showed that better control of blood sugar levels slows the onset and progression of retinopathy.
Diabetic Retinopathy
Diabetic retinopathy has four stages. Mild nonproliferative retinopathy is the earliest stage and begins with the formation of retinal microaneurysms, which are small areas of balloon-like swelling in blood vessels that indicate blood vessel wall injury.
Progression to moderate nonproliferative retinopathy occurs as some blood vessels that nourish the retina become blocked. In severe nonproliferative retinopathy, many more blood vessels are blocked, depriving large areas of the retina of their blood supply. These areas of the retina send signals to the body to grow new blood vessels for nourishment. In the most advanced stage, proliferative retinopathy, the signals sent by the retina for nourishment trigger the growth of new, fragile blood vessels. These new abnormal blood vessels can leak, causing hemorrhage formation and possible retinal detachment which can result in severe vision loss and even blindness. The most common cause of vision loss from diabetic retinopathy is diabetic macular edema which can occur at any stage and results from fluid leaking out of damaged blood vessels into the retina which compromises retinal function.
The best way for diabetics to maintain good vision is to have regular eye exams to ensure early detection of diabetic retinopathy and to achieve blood sugar, blood pressure, and cholesterol control.
Being aware of any changes in vision or new floaters, should prompt diabetic patients to pursue an urgent exam by their retina specialist. If a patient is diagnosed with diabetic macular edema, this can be treated with medications, including bevacizumab (Avastin), ranibizumab (Lucentis), or aflibercept (Eylea), which are administered directly to the eye. These treatments are also being investigated for proliferative diabetic retinopathy, which would traditionally have been managed with laser therapy or perhaps a surgical procedure called a vitrectomy, depending on severity.
Remember, the best treatment for diabetic retinopathy is prevention. Blood sugar, blood pressure, and cholesterol control are paramount in preventing and minimizing diabetic retinopathy. Early diagnosis is also important. I urge all individuals with diabetes to see their retina specialist for a thorough dilated eye exam.

Leave a Reply
Want to join the discussion?Feel free to contribute!